Si-Bo Wang1, Xiao-Cong Wang2, Yan Ma2, Kang-Ding Liu1*, Ying-Qi Xing1*
Abstract
Contrast-enhanced transcranial Doppler (c-TCD) has been used to detect right-to-left shunts (RLS) because it is highly sensitive and cost-effective. The use of provocation maneuvers, such as physiologic maneuvers (e.g., coughing) and the Valsalva maneuver (VM) to transiently increase right atrial pressure and induce RLS increases the sensitivity of RLS detection. In this study, we sought to determine whether coughing is as effective as the VM in aiding the detection of RLS. We evaluated 162 subjects for RLS, using c-TCD under three different conditions: (i) resting state, (ii) coughing, and (iii) modified VM (m-VM), which involved blowing into a tube connected to a sphygmomanometer at 40 mmHg for 10 s. The positive rate of RLS detection with the m-VM was significantly higher than that with coughing. In addition, a difference between the two maneuvers was observed in terms of the degree of RLS seen. The m-VM should be widely used to detect RLS, because it is reliable, standardized, and cost-effective.
Introduction
Right-to-left shunt (RLS) has recently been reported as a risk factor for cryptogenic stroke, migraine, and decompression sickness [1±4]. A previously published study also found that provoked RLS (i.e., RLS that occurs only after a provocation maneuver) is associated with vertebrobasilar lesions in patients with ischemic stroke [5]. Contrast-enhanced transcranial Doppler (c-TCD) is a clinically applicable and reproducible method for detecting RLS, including intracardiac and extracardiac RLS. Provocation maneuvers aim to raise right atrial pressure and increase the sensitivity of RLS detection [6, 7]. These maneuvers are therefore recommended when detecting RLS and in routine clinical practice. Several different provocation maneuvers are used for this purpose, including physiologic maneuvers, the conventional Valsalva maneuver (c-VM), and the standard or modified Valsalva maneuver (m-VM) [8±10]. A simple cough has been used as a physiologic maneuver to provoke RLS [8, 9]. Unfortunately, the most recent International Consensus Meeting did not provide explicit instructions regarding the standard procedure for the VM [7]. In a recent study, authors reported that m-VM provoked a much higher positive rate of RLS detection than c-VM (hold expiration and release to transiently increase right arterial pressure), with higher detection rates observed in c-TCD [11]. These different provocation maneuvers are used in RLS detection tests, including contrastenhanced transthoracic echocardiography (c-TTE), contrast-enhanced transesophageal echocardiography (c-TEE), and c-TCD [6, 8]. The relative accuracy and detection rates of these tests are the source of much controversy and discussion. However, most authors use the VM as a provocation maneuver in c-TCD tests, while coughing and the VM are used in c-TTE and c-TEE studies to increase the sensitivity of RLS detection. With this in mind, we sought to determine whether coughing is as effective as the m-VM as a provocation maneuver for RLS detection during c-TCD.
Methods
Participants
The study design was approved by the Ethics Committee of the First Hospital of Jilin University. We enrolled 162 patients (44 men) with a mean age of 39.04 ± 10.26 years (range, 16±65 years), who were referred to the Department of Neurology of our hospital between October 2015 and April 2016, due to a strong suspicion of RLS. Written informed consent was obtained from all enrolled participants and the methods were performed in accordance with approved guidelines. The individual in Fig 1 has given written informed consent to publish these case details. Of the patients enrolled, 158 had headaches, three dizziness, and one unilateral upper limb numbness. Among patients with headaches, 135 were diagnosed with migraine and eight with tension-type headaches based on the International Headache Society Criteria [12]. Patients with severe arterial stenosis, an insufficient temporal window, inadequate cubital venous access, and those unable to perform the m-VM because of severe heart or lung disease were excluded.
Contrast-enhanced transcranial Doppler
All subjects underwent c-TCD and c-TTE simultaneously, which were performed by two independent operators. A baseline TCD examination was performed with a TCD detector (EMS- 9A, Delica, China). We used a hand-held 2-MHz probe at the right middle cerebral artery (MCA) with participants lying comfortably in the left lateral position. c-TTE was performedusing the GE Vivid E9 platform and M5S transducer (Horten, Norway). Four-chamber views were obtained to optimize visualization of the interatrial septum. An 18-gauge catheter was placed in the right antecubital vein. The medium was prepared by hand by mixing 9 mL of saline, 1 mL of air, and a drop of the participant's own blood [13]. The medium was rapidly mixed back-and-forth with two 10-mL syringes connected by a three-way stopcock 30 times to create microbubbles (MBs). The procedure was performed using three different conditions: (i) RS, (ii) the simple cough maneuver, where the patient vigorously coughed for 10 s immediately after the medium injection [10], and (iii) m-VM. The cough maneuver was determined to be adequate if a leftward shift of the atrial septum was present on c-TTE imaging. For the m-VM, participants were coached to blow into the connecting tube of a sphygmomanometer at 40 mm Hg for a 10-s period, starting 5 s after the initiation of medium injection [7, 11]. After the RS test, patients were randomly assigned to either cough or to undergo the m-VM test first. Measurements were performed twice with the simple cough method and twice with the m-VM; RLS was rated based on the highest number of MBs detected in the 20-s duration of each c-TCD run [7]. There was an interval of at least 5 minutes from the last observed MB between tests. MBs were defined as a typical chirping sound and visually by the spike-like appearance in the frequency spectrum and M-mode. Two blinded ultrasound technicians assessed the prevalence and extent of RLS. Several different categorization systems exist for RLS [3, 7, 14, 15]. Based on standards reported by Jauss et al., Wessler et al., and Xing et al. [7, 15, 16], a five-level categorization system was used in this study based on the appearance of MBs in the TCD spectrum using unilateral MCA monitoring as follows: Grade 0, negative; Grade I, 1 _ MBs _ 10; Grade II, 10 < MBs _ 25; Grade III, > 25 MBs and no curtain; and Grade IV, curtain where a single bubble cannot be identified (Fig 2).
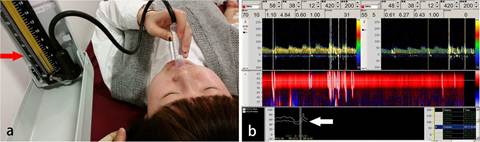
Fig 1. Quality control of the modified and conventional Valsalva maneuvers. (a) The red arrow shows 40 mmHg on the sphygmomanometer. (b) The white arrow shows the Doppler flow velocity curve (down first and then up) (adapted from Guo et al. with permission [11]).
Statistics
Statistical analyses were performed using SPSS 17.0 (Chicago, IL, USA). The0020difference between the detection rates of the different maneuvers was analyzed using the chi-square test. Data are presented as numbers (%). McNemar's test was used to compare the positive rates of RLS detection between the different tests maneuver/c-TCD combinations. Bowker's test was used to compare the extent of RLS between coughing and the m-VM. The level of significance was set at a P-value < 0.05.


